Coxarthrosis is a common degenerative-dystrophic disease of the hip joint, in which, due to age changes or other factors, gradual destruction of the joint joint of the femoral head and the acetabulum of the pelvis occurs. It is accompanied by pain and limitation of the amplitude of movement of varying degrees, which depends on the degree of development. And if in the initial stages it is possible to cope with coxarthrosis with conservative methods, then in the 3rd stage it is possible to save the situation and maintain the working capacity of the hip joint, that is, to avoid disability, only by performing operations.
It belongs to the group of arthrosis and can be accompanied by the development of similar processes in other joints, and this pathology accounts for about 12% of all diseases of the musculoskeletal system. But the term "coxarthrosis" can only be used to describe degenerative-dystrophic changes in the hip joint.
What is coxarthrosis
Coxarthrosis is a complex pathology of one or both hip joints, in which the cartilaginous layers covering the head of the femur and the acetabulum are destroyed, which leads to a reduction in the size of the joint space. As the disease progresses, deformations of bone surfaces and formation of bony growths, called osteophytes, are observed.
Coxarthrosis is the second most common disease of the musculoskeletal system. More often, only gonarthrosis, i. e. degenerative-dystrophic change in the knee joint, is diagnosed. However, the probability of disability in coxarthrosis is significantly higher.
The entire hip joint is enclosed in a special housing, called the joint capsule. It has a so-called synovial membrane that produces synovial fluid. This liquid is necessary for the proper functioning of the joint, because it not only lubricates the hyaline cartilage, but is also a source of nutrients for it.
Normally, cartilage is constantly worn out and immediately renewed due to the continuous regeneration process that takes place with the help of substances that enter it from the synovial fluid. But with injuries or changes in age, the speed of the regeneration process decreases, which leads to the gradual wear of hyaline cartilage and the development of coxarthrosis.
This is due to changes in the amount of synovial fluid produced and its composition. Under the influence of unfavorable factors, it becomes thicker and is produced on a smaller scale. As a result, the synovial fluid is no longer able to provide the hyaline cartilage with all the necessary substances in the right amount, which leads to its rapid dehydration and thinning. The strength and elasticity of the cartilage gradually decreases, the areas of delamination of the fibers that form it, cracks are formed in it, and the thickness also decreases. These changes can be observed during instrumental diagnostic methods, especially the narrowing of the joint space draws attention to itself.
The narrowing of the joint space leads to increased friction between the bony structures that form the hip joint and increased pressure on the already degrading hyaline cartilage. This causes even more damage, which affects the functioning of the joint and the condition of the person, because the deformed areas prevent the head of the femur from sliding easily into the acetabulum. As a result, symptoms of coxarthrosis appear.
If left untreated, the pathological changes worsen, and the hyaline cartilage wears out more and more. After that, it completely disappears in some areas, which leads to bone exposure and a sudden increase in the load on the joint. Since during movement within the acetabulum, the head of the femur rubs directly against the bone, this causes severe pain and severe limitation of mobility. In this case, the pressure of bone structures on each other leads to the formation of bone growths on their surface.
Formed osteophytes can have sharp parts that can injure the muscles and ligaments surrounding the hip joint. This leads to severe pain both directly in the joint area and in the groin, buttocks and thighs. As a result, the patient spares the injured leg, puts less strain on it and tries to avoid unnecessary movements with it. This causes the development of muscle atrophy, which further worsens mobility disorders and ultimately leads to lameness.
Causes

There are many reasons for the development of coxarthrosis, although in rare cases it occurs against the background of the absence of any prerequisites. In this case, they are talking about the presence of primary or idiopathic coxarthrosis. In the vast majority of cases, secondary coxarthrosis is diagnosed, which becomes a logical consequence of a series of diseases or changes in the state of the musculoskeletal system. It can be caused by:
- hip joint injuries of various nature, including fractures, dislocations, bruises, sprains or torn ligaments;
- hard physical work, professional sports, especially weightlifting, parachuting, jumping sports;
- sedentary lifestyle;
- overweight, which significantly increases the load on the hip joints;
- foci of chronic infection in the body;
- congenital malformations of the hip joints, such as dysplasia or dislocation;
- metabolic pathologies and endocrine disorders, especially gout, diabetes mellitus, especially in decompensated form;
- aseptic necrosis of the femoral head, which may be a consequence of a femoral neck fracture, especially during conservative treatment;
- inflammatory joint diseases, including rheumatoid arthritis, bursitis, tendinitis;
- diseases of the spine;
- genetic predisposition;
- the presence of bad habits, especially smoking.
Nevertheless, the main cause of coxarthrosis is still inevitable age-related changes, and the presence of the above-mentioned factors only increases the likelihood and speed of its development.
Symptoms of coxarthrosis

The disease is characterized by a gradual progression with a systematic increase in the intensity of symptoms. Therefore, in the initial stages, it can be asymptomatic or only occasionally cause anxiety in patients, but later the condition of the hip joint worsens, which leads to an increase in the severity of the signs of coxarthrosis to unbearable pain and a significant limitation of mobility. .
Therefore, degenerative-dystrophic changes in the hip joint are followed by:
- Pain of varying intensity, which initially occurs after physical exertion or walking and subsides after rest. The intensity of the pain syndrome gradually increases, it occurs more often, lasts longer and the periods between the moment of applying load on the joint and the onset of pain decrease. Later, the pain is present almost constantly, including at rest, and becomes unbearable. Increased pain at any stage of disease development during hypothermia and lifting heavy objects is characteristic.
- Limitations of the mobility of the hip joint, which are initially manifested by minor difficulties in carrying out rotational movements of the leg. Over time, morning stiffness appears, which disappears after the patient "disperses". This may be accompanied by the appearance of edema in the hip joint. As the disease progresses, mobility limitations become more pronounced and permanent, i. e. they do not disappear after warming up. Patients notice a decrease in the amplitude of leg movements, and after that they completely lose the ability to perform certain movements.
- A crack in the hip joint, which appears when walking or performing physical work, especially when performing extension. It becomes the result of friction of bare bone structures against each other, which is accompanied by a sudden increase in pain.
- Spasm of the thigh muscles, leading to diffuse pain in the thigh. This can be a consequence of various intra-articular disorders, including nerve compression, excessive stretching of the ligaments surrounding the joint, as well as the development of synovitis, i. e. inflammation of the synovial membrane and the accumulation of inflammatory effusions in the hip joint cavity.
- Lameness, which is initially the result of the patient's unconscious desire to reduce the load on the diseased joint and transfer the weight to the healthy leg in order to avoid the appearance or increase of pain, and then the development of muscle contracture. The latter phenomenon occurs already in the later stages of coxarthrosis and leads to the fact that the patient is unable to fully straighten the leg and, moreover, keep it in this position. Thus, the lower limb with the affected hip joint is constantly in a slightly bent position, which causes lameness.
- Reduction in leg length, which usually occurs already in severe degenerative-dystrophic changes in the hip joint, accompanied not only by narrowing of the joint space, but also by flattening of the head of the femur, muscle atrophy. As a result, the diseased leg becomes shorter than the healthy one by 1 or more centimeters.
Coxarthrosis can affect one hip joint, and both at the same time. But if in the first case the symptoms of the disease will be observed only on one side, then in the second they will not only be bilateral, but will also differ in intensity. It depends on the degree of destruction of each hip joint.
Degrees of coxarthrosis
The nature of the manifestations of the disease depends on the stage of its development. In total, there are 3 stages of coxarthrosis, the first of which is considered the easiest. In the initial stages of degenerative-dystrophic changes in the hip joint, only episodic pain can be observed. As a rule, this happens after intense physical effort, playing sports or a long walk. Therefore, patients most often do not pay attention to them, attribute them to fatigue and consider them normal changes in age. In this regard, coxarthrosis of the 1st degree is diagnosed only in isolated cases, which usually occurs during an examination for another reason.
As the disease progresses, its symptoms intensify and are already felt in 2nd degree coxarthrosis. This stage of the development of the pathology is characterized by the narrowing of the joint space by 50%, as well as the appearance of signs of deformation of the femoral head with its displacement.
With further progression of the pathology, the joint space narrows even more, and in the 3rd stage of coxarthrosis, it is almost completely absent. This is already accompanied by the formation of more osteophytes. At this stage of the disease's development, the pain becomes not only severe, but also unbearable and often occurs even in a state of complete rest, including at night. Since the hip joint is very deformed, its elements can affect the nerves that pass through it, which leads to pain that radiates to the groin, buttocks, as well as the thigh and even the lower leg. It also provokes the inability to move independently without the use of aids, such as crutches or canes.
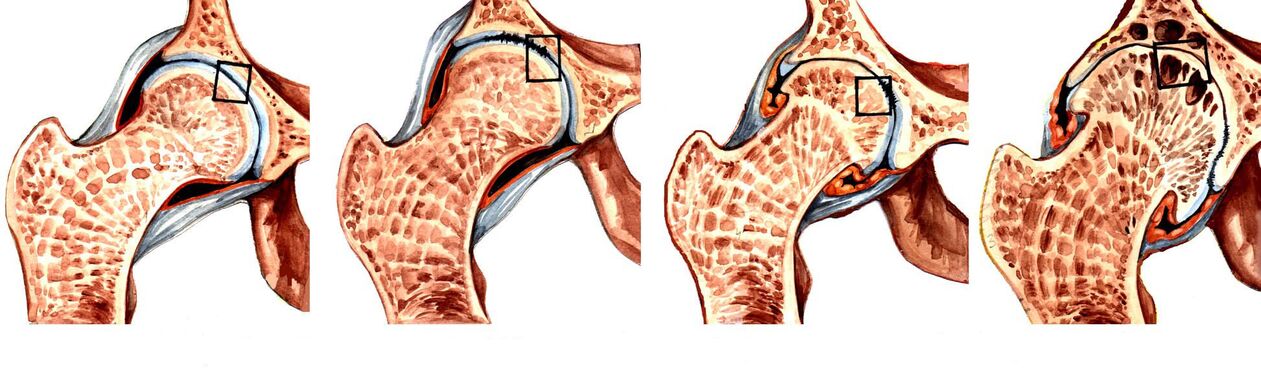
Grade 3 coxarthrosis is a direct indication for surgical treatment. If the operation is not performed in time, the head of the femur will be firmly connected to the surface of the acetabulum with osteophytes. This will lead to the shortening of the leg, the complete absence of the possibility of independent movement, because the joint will completely lose mobility, that is, disability.
Diagnostics
If signs of coxarthrosis appear, it is recommended to contact an orthopedist as soon as possible. Initially, the doctor will interview the patient and determine the nature of the complaints, and then proceed to the examination and performance of functional tests, comparing the length of the legs. As a rule, the obtained data are sufficient to speak with a high degree of reliability about the presence of coxarthrosis.
But since such a clinical picture can accompany a number of other diseases of the hip joints, both inflammatory and non-inflammatory in nature, instrumental diagnostic methods are needed. With their help, the specialist will be able not only to confirm the presence of coxarthrosis, to distinguish it from radicular syndrome caused by spinal pathologies, but also to correctly assess the degree of its development, which means choosing the most effective treatment tactics. .
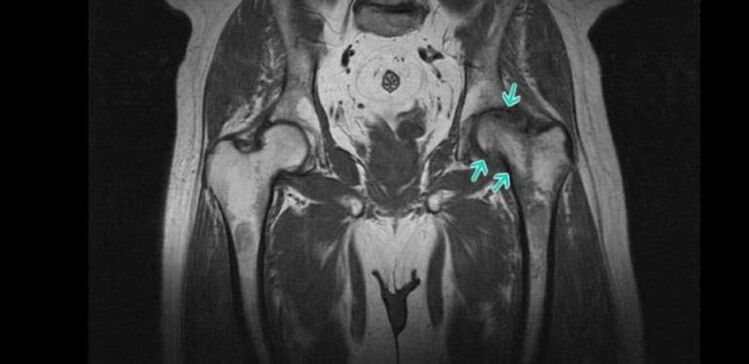
Today, the following are used to diagnose coxarthrosis:
- X-ray of the hip joints - the obtained images allow you to detect signs of destructive changes, the presence of osteophytes, the nature of the deformation of bone structures and measure the thickness of the joint space.
- CT is a more modern method for diagnosing bone pathologies, it provides clearer data than X-rays, but it is more expensive. Therefore, CT is prescribed in controversial cases, when it is necessary to clarify the diagnosis and the degree of destruction of the hip joint.
- MRI is a highly informative method for examining joints, which provides the maximum amount of information about the state of the joint and all its structures, especially hyaline cartilage, ligaments and blood supply characteristics.
Patients are prescribed a series of laboratory tests, including KVA, OAM, rheumatic tests, biochemical blood tests and others.
Conservative treatment of coxarthrosis

When diagnosing stage 1 or 2 coxarthrosis, treatment is carried out with conservative methods. They are selected individually for each patient, taking into account the detected comorbidities. Therefore, it is often necessary to consult not only an orthopedist, but also a doctor of other specialties who will choose the necessary treatment to combat accompanying diseases.
As part of the treatment of coxarthrosis, patients are prescribed:
- drug therapy;
- exercise therapy;
- physiotherapy.
It is mandatory for all patients to take measures to eliminate factors that increase the load on the legs and contribute to the progression of degenerative changes in the hip joint. This includes adjusting your diet and increasing your level of physical activity if you are overweight. If the patient is regularly exposed to excessive physical exertion, it is recommended to change the type of activity or reduce the intensity of training, if the load is caused by sports. In some cases, it is recommended to use special bandages and orthoses that will fix the hip joint and relieve it during physical exertion.
Medical therapy
As part of drug treatment, patients are individually selected drugs, taking into account existing concomitant diseases. As a rule, drugs from the following pharmacological groups are indicated for coxarthrosis:
- NSAIDs - an extensive group of drugs that exhibit analgesic and anti-inflammatory effects (available in various dosage forms, including tablets, capsules, gels, creams, solutions for injections, which allows you to choose the most effective and convenient form of administration);
- corticosteroids - drugs that have a strong anti-inflammatory effect, but due to the high risk of side effects, especially when oral forms are used, they are prescribed only for short courses in the form of injections;
- muscle relaxants - drugs that help reduce muscle tone, which allows you to effectively deal with muscle spasms, which are often observed in coxarthrosis;
- chondroprotectors - a group of drugs that contain components that the body uses to regenerate cartilage tissue;
- preparations that improve microcirculation - help to improve the nutrition of soft tissues and activate the course of metabolic processes in the affected area;
- B vitamins - are indicated for nerve conduction disorders caused by nerve compression by altered components of the hip joint.
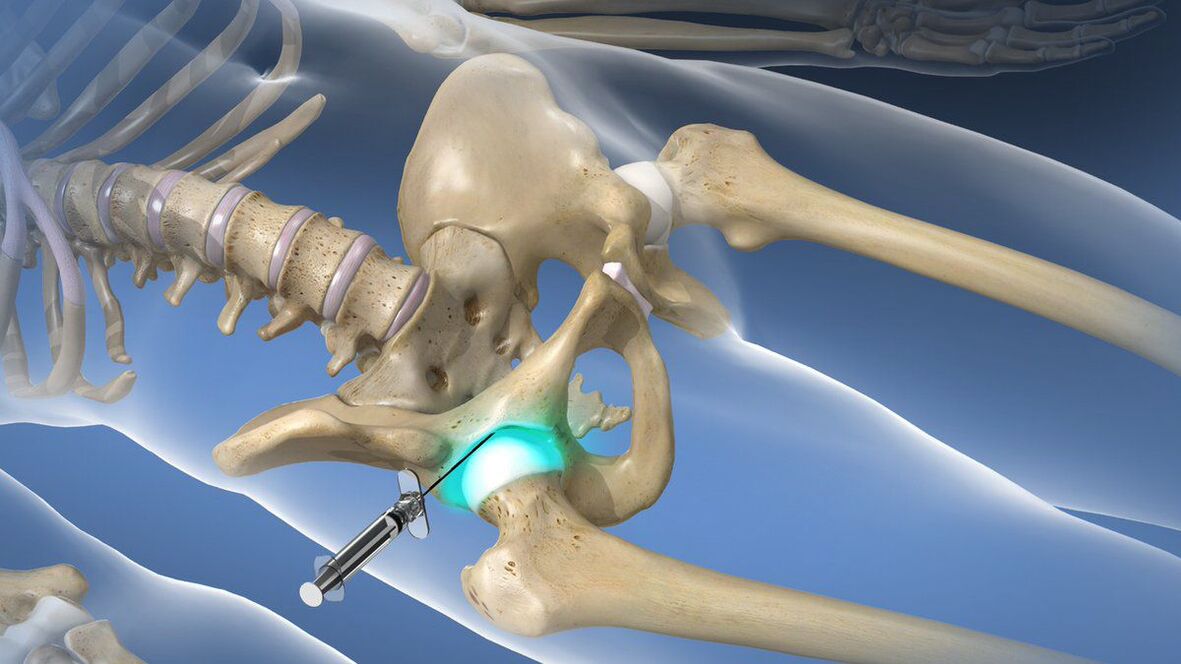
If coxarthrosis has caused an attack of acute pain, which cannot be stopped with the help of prescribed NSAIDs, patients are recommended intra-articular or peri-articular blockade. Its essence lies in the introduction of an anesthetic solution in combination with corticosteroids directly into the cavity of the hip joint. This will allow you to quickly remove pain and reduce the inflammatory process. But the blockade can only be performed by a qualified healthcare professional in a specially prepared room. Performing such procedures at home is not shown.
exercise therapy
When diagnosing coxarthrosis, regular exercise therapy is mandatory. In the same way as drug therapy, a set of exercise therapy exercises for each patient is selected individually, taking into account the degree of destruction of the hip joint, the level of physical development of the patient, the nature of accompanying diseases (special attention is paid to cardiovascular pathologies).
Thanks to daily exercise therapy, you can:
- reduce the intensity of pain;
- increase the mobility of the hip joint;
- reduce the risk of muscle atrophy;
- eliminate thigh muscle spasms;
- they activate blood circulation and thereby improve the nutrition of the affected joint.
All exercises should be performed smoothly, avoiding sudden movements and jerks. But if pain occurs during exercise therapy, you should definitely contact your doctor to correct the selected complex or perform a re-diagnosis to rule out the progression of the disease and the need for surgery.
Physiotherapy

Comprehensive treatment of coxarthrosis includes physiotherapy procedures that have anti-inflammatory, analgesic, decongestive and tonic effects on the body. Therefore, patients are most often prescribed 10-15 procedures:
- ultrasound therapy;
- electrophoresis;
- UVT;
- magnetotherapy;
- laser therapy etc.
Recently, plasmolifting has been increasingly used as part of conservative treatment of coxarthrosis, which can significantly increase the rate of regeneration of hyaline cartilage. The essence of the procedure is the introduction into the cavity of the hip joint of purified blood plasma, which is obtained by centrifugation from the patient's own blood.
Coxarthrosis operation

If the patient is diagnosed with coxarthrosis of the 3rd degree, he is indicated for surgical intervention, because conservative methods are already powerless in such cases. Unfortunately, these situations are extremely common today, because a large number of patients seek medical help when they can no longer endure the pain or have serious limitations in their movement that deprive them of the ability to work and move independently.
Timely surgical intervention can completely eliminate these disorders and restore the patient's ability to move normally, significantly improving his quality of life. Indications for its use are:
- significant reduction of joint space by more than 80%;
- the presence of severe pain in the hip joint, which cannot be eliminated;
- pronounced mobility disorders;
- femoral neck fracture.
The gold standard for the treatment of severe coxarthrosis, including in the elderly, is hip arthroplasty. This operation involves replacing the destroyed hip joint with an artificial endoprosthesis made of durable and at the same time biologically compatible materials. Endoprosthetics allow you to fully restore the functionality of the hip joint, remove pain and return the person to a full active life.
The essence of this type of surgical intervention is the resection of the head of the femur and a small fragment of its neck. Also, the surgeon will have to prepare the surface of the acetabulum for the installation of the endoprosthesis, i. e. remove all formed osteophytes and achieve maximum restoration of its normal shape. After that, an endoprosthesis of the selected type is installed, which is fixed with a special cement (preferably for the treatment of the elderly) or in a cementless way. In the latter case, the endoprosthesis has a special spongy part in contact with bone structures. Its fixation in the acetabulum is ensured by sprouting bone tissue through the sponge.
For each patient, the type of arthroplasty is chosen individually. The most effective is total arthroplasty, which implies a complete replacement of the entire hip joint, i. e. the neck and head of the femur, as well as the acetabulum.
If the patient has preserved normal hyaline cartilage on the surface of the acetabulum, he can undergo partial arthroplasty with replacement of only the femoral head and/or neck. For this purpose, endoprostheses of different designs are used: monopolar and bipolar.
The only disadvantage of arthroplasty can be considered the need to replace the implanted endoprosthesis after 15-30 years.
After replacing the endoprosthesis, the patients are shown rehabilitation, the duration of which depends on the speed of tissue repair. As part of recovery, exercise therapy, physiotherapy and therapeutic massage are prescribed.
Before the advent of modern endoprostheses, patients with stage 3 coxarthrosis were prescribed osteotomy or arthrodesis. Today, these techniques are used less and less, because they have a number of disadvantages. Thus, arthrodesis involves the fixation of bone structures of the hip joint with metal plates. As a result, the pain syndrome is completely eliminated, but the joint completely loses its mobility. So, after arthrodesis, the patient can only stand, but can no longer walk independently due to the lack of movement in the hip joint. Therefore, arthrodesis is practically not performed today.
Osteotomy involves performing an artificial fracture of the femur with such a combination of bone fragments that will reduce the load on the affected hip joint. But the operation gives only a short-term effect, and in the future the need for arthroplasty still arises.
Thus, coxarthrosis of the hip joint is a rather dangerous disease, which can lead to disability. It seriously reduces the quality of life and deprives a person of working ability. But if you pay attention to the early signs of pathology and get advice from an orthopedist in time, you can slow down its progression and achieve a significant improvement in well-being. But with coxarthrosis that has already started, there can be only one solution - arthroplasty. Fortunately, this method can be used even with serious degenerative-dystrophic changes and completely restore the normal functioning of the hip joint.


























